Conversations: With Dr. Andrew Browning, Author & Christian Missionary Doctor
In this conversation, John sits down with Dr. Andrew Browning, an obstetrician-gynecologist who has devoted his life to improving maternal health in Africa, with a particular focus on fistula surgery.
Transcript ShowHide full transcript
Chapters
- Introducing Dr. A Browning
- What is a fistula?
- Maternal Deaths & Training in Tanzania
- The West's lack of gratitude
- Aunt Val & Dr. Catherine Hamlin
- The struggles of remote Africa
- The life Andrew might have had in the West
- Faith & Medicine
- Lessons we can learn from Africa
- The depopulation bomb
- The impact of mission agencies
- The Black Lives Matter Movement
- The Barbara May Foundation
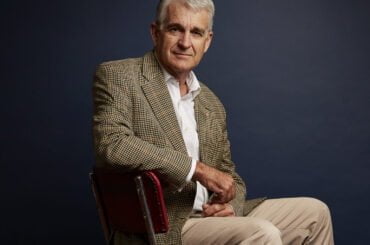
John Anderson: This conversation is with Dr. Andrew Browning. And Andrew has written a book, which I picked up only a matter of eight or nine months ago and could not put down, it’s called a Doctor in Africa. And you’ll see Andrew today like [00:01:00] me in a suit and tie. But he looks very different on the cover of this. He’s in working clubber and as in fact I usually am as well, but his is a medic, mine as a farmer.
And there you go. I couldn’t put the book down because Andrew is a vivid writer. It’s a fascinating story, and unlike so many autobiographies, it’s not about him. There’s an extraordinary modesty about the whole work. At the same time as he tells a story that’s so powerful that no less a figure than Princess Anne wrote a preface for it.
Who’s Andrew Browning? An Australian trained obstetrician and gynecologist who’s worked as a Christian missionary doctor in Africa for nearly 20 years as a senior fistula surgeon. My understanding, he can correct me when we start talking if I’m wrong, but he himself has undertaken something like eight and a half thousand operations.
Transforming, life transforming operations. [00:02:00] Andrew was active in Rwanda during the terrible genocide period. He led the first regional Hamlin fistula hospital and served tirelessly transforming rundown health services into safe and functional ones for poor women in remote regions. He continues to operate fistula camps in Malawi, Sierra Leone, Kenya.
Chad, Uganda, Congo, and Togo. I found him very inspirational, not just because of the book and his profound commitment to using his talents for the benefit of others when so often most of us want to use ’em for ourselves is what lies at the base of my great respect for him. Andrew, thank you so much for giving us your time.
Andrew Browning: Thank you, John.
What is a fistula?John Anderson: Can I begin by saying, look, you frankly have devoted your life to helping women on the other side of the world from very different cultures suffering from the horrors [00:03:00] of obstetric fistulas. Firstly, can you tell us a little bit about what this condition is? I. And what it actually means for the women who have this terrible problem.
Andrew Browning: Yeah. Thanks John. It might be easier to explain what a fistula is by giving you a story of a patient, and I’ve got many stories as you alluded to. I’ve operated on many thousands of women in fish with fistulas and many tens of thousands more of cared for them indirectly. But there are some stories that just stick in your mind.
And I’ll tell you the story of Aldo. Who was a patient of mine in East Africa some years ago, and she was quite typical. She was living in a remote village in southern Tanzania, miles from any sort of medical infrastructure or help or midwives or doctors. So Anglo grew up in a little village she was married at, she doesn’t know the age, but probably about the age of 15.
And soon after became pregnant. She did what all the women in her village did and she went in labor in her mother-in-law’s house. [00:04:00] And I tried to deliver her baby after a full day of labor. She still hadn’t delivered her child. She got into what’s called obstructed labor. And this is the medical part of the talk, John.
Yeah. I actually gave this talk to a boys school just recently, and this part of the talk one of the boys fainted. And so I asked the teachers, oh, should I turn it down? They said, oh, don’t, don don’t worry. He fainted in sex ed class, so you’re all right. But I’ll give you that explanation.
Obstructed labor means that the baby’s just getting stuck in labor. So if this is the mother’s pelvis, baby’s head, It’s getting stuck. There’s a mismatch. Either the pel is too small, head’s too big, or maybe the baby’s coming out the wrong way. It’s getting stuck. So this happened to Anglo, as it does to many women in Australia as well.
But for Anglo, she couldn’t get to a hospital. She couldn’t have a cesarean and operation, so she stayed in labor. Another full day passed and after two days of labor, she still hadn’t delivered her child. The husband [00:05:00] was beside himself. He knew that she should have delivered by now but didn’t know how to help.
He was illiterate. He’d never been to school, but he had the idea that if he boiled some water and put her feet into the boiling water, that might stimulate her uterus to contract. He did this for two more days, and after four days of labor, she still hadn’t delivered her child. She was now unconscious.
And unconscious. On the fifth day of labor, she delivered a dead or stillborn child. It took her two days to regain consciousness, and when she did regain consciousness, she found that she was leaking uncontrollably from her bladder and also her bowel. Because she’d been in labor for so long, the baby’s head had been pressed against the bones of her pelvis.
So all the tissues between bladder, birth canal, rectum, birth canal, all had its blood supply cut off. So those tissues died. So after she delivered her stillborn child, [00:06:00] all those dead tissues came away and she was left with a big fistula or a hole between bladder, outside world, rectum, outside world. She says she was leaking continually.
She smelt. She was ashamed. Husband divorced her. She went back to live with her mother. The mother couldn’t keep her inside the house ’cause she smelt so badly. She was too ashamed to go to church or to the community, so she locked herself away in a little Hutt and unable to walk because of burns on her feet.
She stayed in that Hutt for 18 months. After 18 months, she was found by a mission and taken to a hospital about a hundred kilometers away. They tried to help her. They operated on her three times but she couldn’t be cured ’cause they hadn’t been trained in this fistula surgery, it’s called. She was then found by our outreach workers and brought to us.
In Northern Tanzania, a huge two day journey for her to come to us. And we operate on our patients with a spinal anesthetic, so [00:07:00] they’re awake during the operation. It’s a very safe anesthetic, but Anglo, as we operated, was had so given up hope that she could ever be cured, that she just sobbed uncontrollably throughout the operation.
We operated she had a two week recovery period in the hospital with all the other fistula patients. So she came, she was very demure. She barely looked at anyone in the face. She was depressed. But as in that two week recovery period, she started to interact with the other patients, started to smile, started to laugh.
She saw the catheters come out of the other patients and saw one by one that they were dry and cured. And then it came for her day to have the catheter out. And she was thankfully cured, just rejoicing, giving thanks to God, clapping her hands, jumping and dancing, just giving thanks to God that her dignity was restored.
And she said to me as she was leaving, look, I’m gonna go home. I’m never going to get married again. I’m never going to meet another man. I’m gonna study and become a midwife and help I. Women just like me. So she went home caught up with her a couple of years later and she was [00:08:00] going to school back in her village.
And who knows, in a few years time, maybe she will be a midwife and help women just like her. So that’s the experience of having a fistula is absolutely awful. Women’s. Have been giving fistulas ever since they first started to deliver babies. There’s records of Fistulas way back in ancient Egyptian Times.
Actually, the world’s first fistula hospital is built in New York in 1855. We’ve eradicated them now. And so that first Fistula hospital is now closed ’cause there’s no business for that in America anymore. But there’s still a great need for care for these women, and we think there’s about 2 million fistula patients still waiting for treatment.
Around the world, most of them in sub-Saharan Africa. So there’s still a great deal of work to do. But there’s also, we know it’s prevented ’cause we’ve prevented it here in our countries. We can also prevent it in the rest of the world as well.
Maternal Deaths & Training in TanzaniaJohn Anderson: And as I understand it from your book and from our conversation, people are starting to get the message and you’re, you are seeing that preventative [00:09:00] side start to trip in.
Andrew Browning: Absolutely. It’s paralleled with maternal death rates Mothers still die all too frequently trying to have a baby. He that we measure it in per a hundred thousand deliveries in Australia, it stands of about seven maternal deaths, mothers dying of a hundred thousand deliveries. Many areas of the world in South Sudan where I was just done two weeks ago, it’s still over a thousand.
Deaths for a hundred thousand deliveries. But as you make healthcare available, affordable, that is free women can have access to safe obstetric care. You’ll not only stop them dying in labor and stop the baby dying as well, but you’ll stop ’em from developing a fistula.
John Anderson: Andrew, when you were just 23, in 1993, you were studying to be a doctor.
You opted to take your in-hospital training in Tanzania, which is. Relatively stable by African standards, but very poor. A lot of very disadvantaged people. Other doctors jet off to London or the US if they had the opportunity. Tanzania borders, Rwanda, where there was a [00:10:00] horrific genocide happening at that time. Why Tanzania?
Andrew Browning: It’s a beautiful place to start with, and despite its poverty. The people are absolutely gorgeous. I didn’t know that before going, of course, but I grew up in a Christian household and we were surrounded by stories of mission. I had an aunt growing up in Africa. I had uncles and aunt who were mysteries in various other places of the world as well.
Grew up in a church that supported missionaries. And at the age of six I was sitting in Sunday school in the church hall in barrel on a freezing cold barrel day. If there are. Anything else but freezing cold days in barrel on the bare wooden floor at the feet of this return nurse mystery. And she’s telling all sorts of romantic, wonderful stories of helping people in Africa and serving God over there.
And the, just the wilds of Africa, the animals the different tribes. I was captivated as a six year old. And I guess that sort of childish imagination hasn’t left me. And so at the age of what was it about 22, 23, I think it was had the opportunity to work in a hospital anywhere.
And so I chose that mission [00:11:00] Hospital that lady had returned from in Tanzania. So pat my bags and off I went and experienced what mission life was like firsthand for the first time.
John Anderson: It’s an interesting contrast. I went to Moshi, depending how you pronounce it in Tanzania a few years ago, and I met there a young.
A Tanzanian doctor who’d trained at the Lutheran Training Hospital. It’s one of, I think only three major training hospitals in Tanzania. And he couldn’t wait to get out of Africa. He wa he was engaged to an Australian girl and all he wanted to do was to get out of there. Despite their critical shortage of doctors and come to Australia. But you’ve chosen to do exactly the opposite. So it says something very interesting about your commitment to serving others.
Andrew Browning: I guess that the inspiration when I was six from the feet of that missionary lady was to serve. As a mystery doctor, but it wasn’t until much later when I was actually 14 that I committed my life to Christ.
Took that step to become a Christian, and there was nothing more liberating than to confess that [00:12:00] Jesus says Lord, and believe in your heart that he raised from the dead That really renewed, refreshed. My life. And I wanted to use the, and committed then to use the skills that he had given me, the gifts that he had given me.
I didn’t deserve any of these medical talents or whatever. They were given to me. So I wanted to use those to serve God. And what better way to serve God than to serve the poor. And there’s plenty of poor people in the world. And There’s more p poor people, comparatively needy people needing healthcare in Africa than they there are in Australia. So in some small way try and balance up that equation.
The West's lack of gratitudeJohn Anderson: I’ve often thought it must be an incredibly difficult cultural adjustment when you’ve been out there living in those circumstances and so forth, and you did it as a young man because you came back here to further your training. So you’d seen it, you’d become enmeshed, you’d become excited by it.
At one level, the challenge of making that service contribution, you come back here where. If I can just be critical of mine and your culture for a moment. We tend to take things for granted. We’re not very thankful for what we’ve got. [00:13:00] How do you, how did you cope then with that adjustment and is it still a big adjustment for you? You go backwards and forwards?
Andrew Browning: Yes, it is. Thanks John. Thanks for perceiving that. It’s And I’ve just came back from Africa a week ago, so you probably ca caught me at one of my most critical time. It takes when you’re in that culture and dealing with the very real and tragic issues of life. And then you come back to Australia and everything is so lovely in comparison.
You have, if I could just. Maybe digress a tiny bit. My, my children grew up in Africa and my youngest just the other day said, look, when we lived in Tanzania, we often didn’t have water in the house. We’d have to go fix it with buckets, and we’d have to boil it to have a. You have a bath and that sort of thing.
We didn’t have electricity for great lengths of time, for days on end. There was sometimes food that we didn’t have and or the police would stop us, the road and hassle us. But I was always grateful for everything. But here in Australia, we always have water. We always have electricity. The police never stop us.
We always have food, and I’m no longer grateful for anything. And he was actually just about 10 when he [00:14:00] said that. Very insightful. But I feel that too. When you live. In a culture. And I’ve lived with some of the most underprivileged cultures. If you’re talking materialistically, talking spiritually, they’re very privileged.
But materialistically mostly some of the most unprivileged countries, peoples in the world. And you come back to Australia where everything is just given to you. People just lose their sense of gratitude because it’s just all, all there for them. And if I was to be critical, that’s the biggest.
Culture shift going backwards and forwards. The lack of gratitude for everything that we do have, but people work for it hard here. There’s no doubt about that. They really do work hard to get that and but a sense of gratitude for that would not be go astray.
John Anderson: Yeah. My family often uses a hacking phrase. Probably everybody’s heard, but we’ll be discussing what looks like some terribly serious problem, and then somebody will just break the ice by. By saying yeah, this is a first world problem, isn’t it? But and just building on that I took my family, ’cause I wanted them to see how fortunate we [00:15:00] were.
We had four kids to Tanzania. And my, at that stage, 12 year old daughter, we went from Tanzania to London and we were walking in Hyde Park and I said to my 12 year old daughter who’s very perceptive,
Yeah, very different, isn’t it? And she said, yes, dad, it sure is. We’ve been in Tanzania where they have nothing and they laugh and they smile and they interact.
And here in London, people seem to have everything and they all look miserable. It really struck me. Very interesting thing out of the mouths of children sometimes.
Aunt Val & Dr. Catherine HamlinJohn Anderson: Now many people in Australia anyway will have heard of Dr. Katherine Hamlin, the Australian doctor, her husband, I think Reg was his name.
That’s right. They started this work and became well known. You got to meet her, I think, and I think she interacted directly with you and asked you to pick up her work. Is that what happened?
Andrew Browning: Yes. So I, to explore missions, I went and in 1996, I think it was, I went to Ethiopia to work with my aunt.
She’s been living there since [00:16:00] 1973. She’s quite a legend, I gather. Val. Yes. She’s the black sheep of the family. And she’s extraordinary actually. She’s married into a nomadic tribe in the desert. She runs a huge development organization employing 750 people bringing literacy work. When they, she first went there The language of the afar wasn’t even in writing.
So they had to put it in writing first, then teach people how to read and write. Then they suddenly realize, oh, there’s no books or newspapers or anything written in afar. ’cause it’s been in writing before. So then they had to put material into writing to give people things to, to read. And so she developed up this huge.
Development organization. And so I went to work with her in the desert in 1996 to explore if we could I could join her as a doctor. And we were wandering around the afar, desert with the nomads, with the donkeys not the donkeys, the camels sleeping out in the desert at night. And it was so hot is the hottest, inhabited place in the world.
And. Come time to, to go to bed, everyone would be in these dome shaped huts. It was about 30 degrees, 35 [00:17:00] degrees, and they think it was chilly at that time of the year. So they had a, an open fireplace in the Hutt. Ooh, 10 of us crammed in these little huts. It was just too hot for me, so I slept outside that Hyen has come.
And prowling around the houses. So I had to sleep with a guard next to me, and every now and then, there’d be a bang, bang as he shoots this clash in the cough. At this high end of getting too close, this yelping high end running away. And then later that nighttime, a camel bellowing belling away, gives birth about two meters away from my head, just splashing me with amniotic fluid.
And I thought, oh my goodness, this life in the desert is. Just bowel. You can have, it’s perhaps not for me. But at that time I visited Catherine Hamlin, a fistula surgeon in Sababu. The capital city of Ethiopia. And whenever I was back from the desert in the city, Catherine would ask me to come to theater with her, ask me to lunch.
I met the fistula patients, absolutely fell in love with ’em. And I thought as a surgeon I wasn’t a surgeon at that stage, but this is how I would love to spend my life by helping these women. And when I left Ethiopia that time, I was going to bed [00:18:00] as of flying in the morning, and Dr.
Hamlin rang me at vows. House in the, in Aaba and she said, look, I’d like you to come back and work for me. And I said, yep, sure. I’m just about to go back to Australia and study theology for a year. Can I pray about it for a while? And so after about four months of praying, I, said initially said no, but felt so convicted that was the wrong decision.
I immediately turned around and said yes. And Accepted the job. And later after finishing obstetrics training moved out to, to work with her. So I worked with Catherine for 10 years in Ethiopia before embarking off with work elsewhere.
The struggles of remote AfricaJohn Anderson: In a, on a continent like Africa, it varies from place to place. I know, but a lot of places you don’t have a lot of internet, which we take for granted. And some places probably don’t even have mobile phone coverage or fixed lines. How do you find the patients in need and how do they find you? How does that work?
Andrew Browning: It’s really hard. Actually, when I first went to Africa in the back on the Rwandan border there, as we were talking about before there was no phones.
It was well before internet and so there was the old postage system. And so it would take three weeks to send a letter and [00:19:00] at best, and three weeks to return one. So it was a six week turnaround time with communication with with the world. But now, last night I was getting calls from Tanzania WhatsApp messages, straight away.
But in the villages These women are still very poor. They’re illiterate, so they can’t read the messages on their phones if they were to receive a text anyway. But they can speak on phones if they had them, if they had coverage. Define the fistula patients is really tough ’cause they’re often hidden away in the village.
They’re ashamed, they don’t want to go out and mix. So it’s actually takes a lot more effort and more expense to find and bring fistula patients. More money is spent on that than actually. The operation itself. Really? Yeah. So we have teams going out, village to village trying to find the patients, and then when if you are, think of, think if you are a literate.
Girl in the remote areas of Tanzania and speaking, you are speaking with your father who’s is quite a patriarchal society. You need permission from your father or your husband. If your husband hasn’t left you to go with some [00:20:00] strangers, halfway across the country, who knows if you’re ever gonna be to see her again.
So to convince them and to get their trust is difficult. Just this two weeks ago, I was, a week ago, sorry, I was in Tanzania. We had one patient who had delivered. After a four day labor dead child, and actually the husband died of a chronic illness, pretty much the same time. So she was back living with her father and she was lost a lot of blood.
She was got infected, she was losing a lot of weight, she was dying. And they saved up enough money to take her to witch doctor in the neighboring village. And actually our outreach team was in the area at the time they heard of this lady and they actually intercepted her on the road to the witch doctor.
And they gave us some medicines. They gave us some iron, gave us some fluids, and said, we’ll be back here in three days. We could take you back to Arusha, to our hospital there and treat you of our fistula if you want. So the father was so impressed and that she saw her. He saw her getting better on the antibiotics and the iron tablets and so forth.
So after two or three [00:21:00] days, the team came back, the father-in-law said, yep, we trust you. She’s getting better already. We didn’t even go to the witch doctor, didn’t spend any of our money. She’s already getting better. Thank you. And so we took her to the team, took her to Arusha. We were operated on her about 10 days ago, and I got news from her, actually, this is one of the calls from Tanzania last night that she’s doing very well and the catheter comes out in about two days time.
And Yeah, I’m sure she’d be cured and be able to rejoin her family.
John Anderson: Fantastic. In Australia we used to, I don’t know whether people even use the word now, but out in the bush where I live, we used to talk about the bush telegraph. Word travels very quickly. Yeah. Presumably when the family, the village, the community, see.
This amazing and miraculous turnaround that in itself builds confidence, builds understanding, builds a desire to do things better.
Andrew Browning: Yeah, the bush telegraph is marvelous. A third of our patients do come because of word of mouth through other patients. Yes. And then a third comes from our outreach team going [00:22:00] from door to door in the villages and then third comes referred by other health centers and so forth.
So the bush telegraph, works tremendously. But the biggest thing with the bush telegraph is to try and convince people to deliver. In hospitals and get to a hospital to have your baby to stop them from dying and stop them from getting fistulas. And so slowly that message is getting up.
More hospitals are getting built by the governments of these countries staffed, although it’s very difficult to staff and train the people they’re making progress. And so we’re slowly, we’re seeing a decrease in the number of home deliveries. So when I first lived in Ethiopia, the home delivery rate was 96%.
So there’s so few hospitals, but now it’s down to around 70%. So moving in the right direction. Some similar statistics with Tanzania, not quite as dramatic. So yeah slowly progress is being made.
The life Andrew might have had in the WestJohn Anderson: I’d like to go back to, this is such a big thing for us to get our minds around that you, you have done something that a man of your talents would not normally do.
You could have been a very [00:23:00] wealthy and a highly sure. You may be these things respected and listened to, senior leader in the medical circles in Australia and traveled the globe lecturing and all of those sorts of things. You’ve chosen not to do that, and you’ve found purpose and meaning and excitement and real enthusiasm.
It just comes through in what you’re doing. That’s terrific. Nonetheless. Your wife Stephanie, who’s an Australian, and a gifted teacher and translator who’s had her own work and her own niche but you’re married overseas. You’ve worked overseas. You, your two boys came into the world overseas.
I. Have you ever doubted that was the right thing to do for the boys? Has that been an issue of playing in the back of your mind? No.
Andrew Browning: No, not at all. My wife grew up in Tanzania. She was a missionary kid herself, and she had 18 years growing up in Tanzania. She only came to Australia three times in those 18 years.
Then we were married in Ethiopia and for our boys I guess it boils down to is what you want to instill. Into your children. Do you want to instill a [00:24:00] comfortable life here in Australia of all the trappings that, that may give to young children? Or do you wanna model a life serving God?
Which I would hope to aspire to and. Expose them to, to a life of service and give them, instill in them a sense of integrity a sense of purpose, a sense of service, and hopefully that’s coming through to our children. I have to pray and trust that to God. But a life in Africa was very rich very enriching for them.
They speak different languages, they’ve experienced different cultures. They’ve. William’s best friend that he still prays for every night is an orphan boy from Ethiopia. And he now communicates with him on WhatsApp. And you mix and deal with all sorts of different people in their lives.
They had a life that was so free in Africa playing just you open the gate of the house and you’re immediately surrounded by 20 boys. ’cause you are the only kid in the ball, the street with a ball. So you’re out playing soccer just on the streets all day, running around. They had a very free, very rich Life in Africa and they still, they’ve been back in Australia for five [00:25:00] years now.
Even last night both of ’em said, oh, we missed Tanzania.
Faith & MedicineJohn Anderson: You mentioned in your book the old adage that God does the healing and the doctor gets paid. I’m not sure that you did get paid very much, but here and there but there are times when you look back, you’ve done an operational, what have you, and you think, oh, I don’t know how this is going to go. But there’s been a really miraculous, really extraordinary sort of shock when it’s come.
Andrew Browning: In in medicine we are fooling ourselves really. There’s very little we can do to cure people of illnesses. We can’t cure, for example, blood pressure. We can manage it.
We can’t cure it. There’s very little that us as very, we think we’re very clever doctors can actually do with the body. And I, there’s been some miraculous things. I. I can’t help but think it’s just the infection of God. I’ve just got no other explanation for it. I am a scientist.
I do rely on my knowledge as a scientist, as a doctor to, to treat and to do my best, but sometimes I’m just completely astounded by what happens [00:26:00] in the body. For example, there was One lady in Sierra Leone she was coming post nasally to the clinic. I was working in Sierra Leone at the time. She delivered her baby.
She was coming for a check, and she had high blood pressure, which is a bit of a risk for things going wrong. And she was in the waiting room sitting next to her husband. And the name, her name was called. And she didn’t move and the husband looked at her and didn’t move, and she was actually dead.
And they asked the husband, oh, how long has she been like this? And she says, oh, she hasn’t been talking for the last half hour. And so we rushed and got her onto the resuscitation table, resuscitated her. It took us about 20 minutes to get a faint little heart rate back. Tried, intubated her, extubated her.
She took a few gas, died again. Heart stopped breathing, stopped. Resuscitated her again for another 40 minutes. Got a faint heart rate back, a couple of of deep breaths. Gas of breathing. That was it. After about an hour and a half of resuscitation, usually after resuscitating you, you give up after half an hour or so.
We don’t know how long she was dead before we started [00:27:00] resuscitating. What kept you going? Oh, just the hope. Yeah. It’s very hard to stop. Yeah. You just want to hope you wanna pray. So we, it is now late at night. We we pray it was in the evening. We said let’s call it, we’ll have to stop. Even if she survives, she’s gonna be so incredibly brain damaged.
There’s no life for her here in Sierra Leon, and we, this is impossible to support. So we prayed for her, left her. We all went about, about our duties. I came back the next morning and fully expecting to hear that she had died in the night. ’cause we left her. She had a faint heart rate.
She was taking the occasional gasper breath. Anyway. She was sitting up in bed talking to her husband. Good grief. Yes. Absolutely down. I just can’t, nothing would ex explain that. It’s just extraordinary. We couldn’t do a thing. God, he’ll, that’s the only explanation I can make. I can say.
John Anderson: Interestingly, at a time when faith is in being pushed to the corners, really in Western society, that’s not true in Africa, is it? There’s an old saying that Christianity’s a mile wide and an inch deep sub-Saharan [00:28:00] Africa, perhaps an estimated 500 million. I’m told people with some sort of nominal attachment, at least to Christianity.
But would you say that you are seeing a deepening of people’s un faith and understanding when they come into contact with the sort of work that you are doing?
Andrew Browning: Oh, absolutely. That’s deep in my faith. I would say I’ve learned much more from them than I’ve imparted to I’ve, yes, I’ve learned much more from them than I’ve imparted to them.
And that’s the sincerity and the depth of their trust in God. As missionaries, I was there as a missionary serving God, and they welcome missionaries. They’re a very religious society. And they’re not suspicious of people professing a faith. They welcome discussion. They love to discuss, my Islamic colleagues and friends up in the afar, desert, that’s 99% Islamic area.
I’ll pray for the patients. Pray to Jesus for the patients before we operate. They’ll join in those prayers too. They’ll have their morning prayers. Yeah, we. We share and we, and it’s religion and the faith [00:29:00] is just part of life. And it’s a very real part of life. And I think it’s partly due to necessity, partly due to poverty.
When you don’t have anything in this material world, you just cry out for something more, you’re looking for something beyond. What in the here and now. And so that’s very real in the communities that I live and work with and have lived and worked with over the last 20, 30 years or so. And it’s a real deep and enriching and a lovely environment to be in.
Lessons we can learn from AfricaJohn Anderson: You, you’ve hinted a bit, Andrew, at what we can learn, what you’ve learned, and what we can learn from our interactions in some of these less fortunate places. We send experts all over the world to teach them what we know. And in part that’s what you are doing. You’re taking Western medical knowledge in there to great benefit, but can you just draw out this idea that you’ve learned a lot from them?
Because I think often we’re a bit patronizing. Oh, and you’ve alluded to the fact that we go in there and say, we’ll help you if you do X, Y, and Z and deny them agency, and they [00:30:00] feel that they’re being colonized again. What can we learn? From
Andrew Browning: African people in your view? I think there’s so much we can learn from each other, isn’t there?
But that learning takes a long time to, to develop that. You can fly into, to these countries and I see it over and over again. A group of experts fly in, they demonstrate some new technique or they come in with a kind of superior attitude. We know what we’re doing here, you do this.
But it’s interesting that about 90% of the research in medicine happens in Europe and America, and it’s in that context, in that pathology, in that populations. But then you apply that to the majority of the world and it doesn’t translate very easily. So I’ve had to do, as a doctor in Africa, I had to do a lot of learning from them.
Of how to handle these diseases in those contexts. ’cause they do present differently. They do. The management is often quite different as well. The context is different. Yeah. There’s so much I could, I’ve learned as [00:31:00] a doctor from them to start with. But as a human, I’ve learned far more from them.
Just, and there’s so much more we can learn from them as a continent, how to be satisfied by and happy living the simple life, how to be content not just. Grabbing more things by building up our life with consumerism, but just to be content by just with a few positions to be happy, not to be so task driven all the time and relationships.
Relationships. The community ties and the family ties are so much stronger, and I think that leads to far greater happiness in life. Research shows, I don’t think you need research to show it, but common sense shows also that, if you’ve got strong communities, you’ve got strong family ties.
If you got if you’re generous with other people, if you help other people, you’re far happier than if you are living the individ individualistic. Life that the west espouses with your individual rights. But if you live in a community, you’re much, much happier. [00:32:00] But if you look at there’s all these world happiness scales and the happiest country in the world is Finland, apparently.
But if you look at how they measure it, it’s g d p per capita. It’s life expectancy. It’s access to social services. It’s all things that of course, Africa Miss misses out on. But even if my children. Noticed, I said, what’s the biggest difference between Africa and here, and your child noticed too?
People in Africa are happy. And ’cause they’ve got those community ties. You don’t put your child into a child daycare and pay a stranger to look after your child the whole day because you’ve got a village there looks after your child. It’s with them, it’s interacting with ’em. The people that they love, they know it’s being cared for and a very real way.
And we’ve missed out on that. In the West, there’s a lot that we can learn from Africa and just of how, what the important things in life are and how to be happy. And they do have a good time. I just recently in Uganda and I was there on a Saturday, so I walked down to the local football field just to watch a game.
It was just a party. It was so much fun. The football field was on the slope like this. They had a huge [00:33:00] anthill in the middle and, but there was guys playing in the mud. Half of them didn’t have shoes. Everyone was shouting and cheering and having a. Great time. One guy got off, he stripped off his shirt and got off and had a kick of the ball, kind of like a pitch invader, and everyone was laughing and cheering him and there was chickens running across the field.
It was so much fun. But I went to a soccer game in on the central game my son was playing, and oh, it was. It was completely different atmosphere. The parents were taking it very seriously. Living their lives through their children. Yeah. Living, shouting at their children. It did, it wasn’t much fun at all.
They really do know how to enjoy life and that’s and the important things in life as well. That’s one thing that we need to learn from them. That’s one thing they need to share with us in the West.
The depopulation bombJohn Anderson: We know that, in fact, contrary to what many people think is happening around the world, we have a depopulation bond going off in many parts of the world.
China leading the pack, their populations in free fall or beginning to go into free fall even Australia, 92 countries population coming down. We also know that African and certain parts of the Middle East [00:34:00] population are increasingly and so a billion people roughly in Africa today. Experts say it may be as high as three, three and a half billion by the end of the century.
I wrote with two others an article for a leading paper in Australia a few years ago pointing to the value of improving nutrition. And for people who are not in disadvantaged around the world, and we’ve done a striking job of it, I have to say we’re feeding another 5 billion mouths every day now than we were over what we were 50 years ago.
A number of stunted children, malnourished people, and so forth, it’s come down dramatically. But I was really, there’s no other way of putting this. I was really taken aback. Pretty offended actually by the number of people who wrote in and said, oh don’t go about this business of saving people’s lives.
We’ve got too many people on the planet. Let them die. Actually, in a pragmatic point of view, I would’ve thought in Africa if a husband and wife or even just a wife are thinking, I’m gonna be able to [00:35:00] deliver babies safely, and they’ll grow up and they’ll be, I won’t lose ’em. Then I won’t have as many children anyway that, in fact, the answer is to lift the, their standards of living and get them into some decent sort of health and even social security parameters, a much more compassionate way to achieve the objective of avoiding, if you like, overcrowding, if that’s your objective or overpopulation in Africa.
Andrew Browning: Now you already see that, the rising middle class…
John Anderson: Can I ask, do you get people making that? Why are you saving these lives?
Andrew Browning: Oh, absolutely. Yeah. All the time. And I’m continually shocked. By that I mean it’s a heartless. Like devoid of any sort of compassion or humanity. And if you had that person in your arms dying, gasping, dying of hunger, dying of thirst as I have how can you ignore them and say, look, your life’s not worth it.
My life’s much more valuable than yours. What kind of attitude is that, certainly from my Christian viewpoint, where we’re. We are [00:36:00] inspired to love. We’re told to love. We can’t help but love when you’ve committed your life to Christ and know his forgiveness and his refreshing spirit. Just you just love and you can’t let that person go. You serve them and you want to do the best by them, but so that, that let those people die is just I can’t comprehend it.
The impact of mission agenciesJohn Anderson: I met a South African, a white, very wealthy man. Yeah. And he wanted to, he thought perhaps I could help he mocked his own sort of sense of superiority. Yeah. So he took his private jet into a refugee camp in Africa, and the plane broke down his own private plane. He was caught there for three days. Great. Yeah. And he described. This was in Cape Town when I was there a few years ago. Yeah. The experience of having a mother coming up to her crying her eyes out, saying, can’t you help me, my baby’s dying of starvation.
Yeah. And handed the baby over and he said, I’ve got this baby in my arms and it dies in my arms. Yeah. And he said it was a life transformational moment. Absolutely. And he started a massive program for feeding AIDS orphans in America, [00:37:00] in Africa. Wow. Staggering number of people. But there, he was a very privileged white man by his own definition. And a baby dies in his arms.
Andrew Browning: Yeah. Maybe that’s it. Maybe it’s just because they haven’t had that experience, but they haven’t been confronted with those situations directly. They haven’t met those people suffering and held them and spoken to them and looked ’em in the eye that they have that reaction.
John Anderson: You’ve pointed out that 50% of the healthcare, in Africa is provided by mission agencies, which is pretty astonishing. Particularly when you think, actually, to be fair, there’s a lot of other people trying to help as well, but it’s still 50%. What would happen. Because many of people in yours and my culture would say, oh, what are these?
Do we still have missionaries? Shouldn’t we have got rhythm by now? What happens if they withdraw?
Andrew Browning: Yeah, they’d still provide a significant, faith-based or church hospitals still provide an enormous amount of the healthcare for Africa, variably put between 30 to 70%. So most quotes put it at around 50%.
So 70% of. DRCs Healthcare was provided by [00:38:00] missions. So it’s extraordinary. And that’s counted by the number of beds that are provided to health to serve the people. And it’s the tr mission, tradition. Hospitals, Christian Hospitals, hospitals, public hospital systems bore out of the Christian Church way back in the Roman times when the Council of NAIA said, look, we’re gonna have to have a place to treat poor people sick people in every Cathedral city.
And so the sisters. We’re also the nurses, so hence we call ’em sisters from the cathedral. So the is that where it came from? Yeah. The idea of calling nurses sisters. I didn’t know that. I’d never heard that. Yeah, so that’s why they called, they were the original out of the monasteries.
Yeah, that’s right. So they yeah, so out of the Christian tradition, the public hospitals started and so as. Africa opened up missions, went there to teach, to, to educate to provide healthcare, to care. And so they’re still there. And we, I. My organization now, the Barbara Ray Foundation is not strictly a a mission, but it’s very much faith-based and we get a lot of our our funding through churches, through like-minded Christian people to be able to do the work that we [00:39:00] do.
We also get funds from secular organizations, non-Christian organizations, who trust and believe in what we do. And the government asked us to build hospitals to to develop their own health infrastructure in a particular area to help train their staff ’cause they’re. They’re making great progress.
There has been an enormous amount of progress in the last 20 years with healthcare for a lot of these countries, but there’s still a lot to do. And so it’s still very much a partnership between the church and between the governments of these countries. And so if Christians are to withdraw, I can’t imagine they would withdraw because it’s not the nature of Christianity.
You serve and do the right thing. But if they were, that would leave, still leave a huge hole. In not only the health system, but also the education system for a lot of these places.
John Anderson: Unlike Christian mission agencies and organizations many western organizations the eu and so forth, frequently make their aid conditional on advocacy around democracy, LGBT, [00:40:00] advocacy, access to abortion and so forth. Do you have any thoughts on the sort of cultural effect of the West’s insistence that they follow our values in a way that perhaps doesn’t respect their own agency? Because some people would say the Christians are trying to influence ’em. To deny their own culture.
Andrew Browning: Yeah, that’s right. I’ve heard of that a lot as well. But as I said before, generally the Christians are welcome. The missions are welcome because they are a religious culture a faith-based culture. And we’re welcomed with open arms. It. Often when I go into a place they, I might meet someone, they say, ah, you with the un?
I said no. Are you with the embassy? No. Oh, you a mission? He said yeah, I’m a missionary. And immediately the atmosphere just. Dissolves into one of familiarity and welcome which is lovely. And because you are been living with the people you’ve learned, I’m hopeless of languages, but I’ve learned some language.
But you’ve served them you’ve worked alongside them. You don’t live in a great big house and have a huge [00:41:00] salary much, much higher than theirs. You try and identify with the people much more and they recognize that as freely given love and. That breaks down all sorts of barriers, and it’s a lesson that I learned very early in my career.
One of my first major operations I did as a fistula surgeon was a lady who was from an area of Ethiopia. I. Islamic area and she had a fistula of course, and she didn’t speak my language. She didn’t have know my religion. She didn’t know my culture and I didn’t know hers. We really had absolutely nothing in common, and I’m sure if we talked to each other there wouldn’t be much that we could agree upon.
But I wanted to help her. I felt compassionate for her. I think that was God given and. But see, her injuries were so dramatic. There’s nothing that anyone could do to cure her. She was one of the few percent of ladies that are beyond cure the bladder’s been destroyed. The birth canal’s completely destroyed.
You can reconstruct as much as you can, but there’ll still be, I. Leaking some urine. And so I did [00:42:00] my best, but I had to talk to her after we removed the catheter and she was obviously still wet. And I said, look, we’ve tried everything. I’ve done my best. But there’s, I was almost in tears, just, it was my first patient that I couldn’t cure.
And I said, look, but we can’t cure you. We’re gonna have to find ways to help you live with this condition. And she just looked at me and said, through a translator, she said, Out of all the people I’ve met this place and this hospital, all my people, they rejected me, all my family, they rejected me.
You’ve come here, I’ve come here, you’ve put your arm around me and you’ve helped me to stand even when no one else would come near me because I felt so badly. You’ve helped me on and off the operating table. You’ve helped me get out of bed. You’ve loved me, and that’s enough. And so that’s a simple thing by sharing love is what we try and do as a Christian.
And it changes lives, it changes cultures, it changes people as Christ’s love for us changes us and to, to a life that serves. But yes, a lot of aid is conditional. Even donors. I went to one of the four major banks here in [00:43:00] Australia recently, trying to get money out of them. And It became evident that their charitable giving was to help youth get jobs as long as they opened an account with ’em.
So I thought, this is not giving, this is just investing. So it was always something conditional. And likewise for the big donors, they come into countries now and they say, you must do this, otherwise we won’t give you the money. And to quote a a good friend of mine who’s actually was the professor of Geography at Dussel Army University in Tanzania.
And very astute man, fully aware of the politics that’s going on. He said it’s, we are seeing it now as just a form of neocolonialism a a form of imperialism. Wow. He actually used the word a very strong word. He said it’s a new slavery. Wow. He said the West imposing their values on us when we don’t want those.
Is a form, he called it slavery. Very interesting and strong remark. He said, A lot of governments now are saying, look, keep your money. We’d rather be poor than accept your imposed values. Yeah. [00:44:00] And that’s right. You can’t change culture. You can’t change people at the point of a gun.
You can’t force people. You can defeat people. You can enslave people, but you can’t win people. And I think that’s the difference between the Christian message, the Christian core essence is to, is Christ’s love. And that wins people. It persuades people. It attracts people. And that changes people.
The Black Lives Matter MovementJohn Anderson: I have to ask you because you’ve been involved in this work of restoring the dignity and the hope for Black African women by and large, and by extension their communities. We’ve seen a lot of protests, sometimes pretty ugly in the West, ostensibly in the name of attacking racism under the Black Lives Matters banner.
Now that was avowedly Marxist. We know that. I can’t help wondering. Whether people can see the contrast. You won’t like me saying this between somebody who walks the talk and someone who just does the [00:45:00] talking.
John Anderson: You may not wanna respond to that, but I’m gonna make that observation. Alright? What you’ve done is a great challenge and a good challenge if you really care. Then go and do something. Yeah, absolutely. Yeah, they are. Or contribute to those who are. Don’t burn down businesses in an American city.
Andrew Browning: No. Your tool is love. And if you really value black lives or any life for that matter yeah the tool is genuine, sacrificial love.
The Barbara May FoundationJohn Anderson: So you returned to Australia during 2008 and started did you start, or you were involved at the start of the Barbara May Foundation? Two things: What is it and in particular, you are obviously seeking to expand the reach and the work and the number of facilities across Africa. Can you give us a feel for those two and how if people really say Black Lives Matters, they can help you? Help others or be involved?
Andrew Browning: Yeah. So up [00:46:00] until I came back for a break in 2008 and did actually some training in plastic surgery to reconstruct, learn how to reconstruct things more properly. And while back in Australia, I, we started the Barbara May Foundation. Up until that point, I’d been operating on up to 600 fistula patients just myself every year and training others and so forth.
And so every day, that’s a couple a day. You don’t operate every day, but yeah. So some days you’re doing, yeah, some days you do eight, some days you do none, but but every story is a heart wrenching story of loss, babies dying, of loss of dignity, and that it’s preventable. I’ve been with a ham, Catherine Hamlin, for those years, up until 2008.
She was busily doing the fistula work in Ethiopia. I wanted to take what I’d seen in Ethiopia to the rest of Africa. And also to prevent it. And we prevent it just the same as we prevented it in America. Put the first fistula hospital in New York, had business by by building maternity hospitals, by enabling women.
To have safe access has to be free because these women can’t [00:47:00] afford it. And has to be safe and accessible. So by building maternity hospitals where there aren’t maternity hospitals. So to do that, I needed a fundraising. Entity. So we started the Barbara May Foundation and launched that in actually 2009.
It it was tough work, starting something new and takes a lot of perseverance and I would say a lot of intervention by God, by blessing us just at the right time in the right way, but slowly. We’re spreading the work and it hasn’t just been me. There’s other organizations doing it as well.
There’s, so Barbara May Foundation is partnering with several other organizations to reach this objective. But slowly we’re like to think we’re making a difference in you some women’s lives.
John Anderson: Now, I know that you’ve done fundraising here in Australia. I know that you’ve also done it in America. Do you get people who have been successful in life and are well resourced?
Andrew Browning: Oh, absolutely. And were very grateful. Yeah, immensely grateful. And it’s always seems to come, not because you look for it, but because is volunteered. Yeah. So nine times out of 10 I look for funds. I go [00:48:00] out and write proposals.
I meet people I. But it’s really the unexpected places that God blesses you with the funds to be able to do it. So actually now we’ve got miraculously we’ve got funds to build two new hospitals, one in Tanzania, one in Uganda. We’re very grateful for that. Both from family foundations and now we’ve got to raise the money to run them.
Of course. That’s the difficult thing. Running cost is an ongoing issue and something that we have to work tirelessly on all year round every year. What will those hospitals look like? We’re used to enormous hospitals that take you forever to wander around and yeah, you don’t corridors for miles.
And I like to build small containable things and I think it works. Much better if you have a staff. We have a staff of between 50 to 70 in our hospitals. And when you have a staff like that you work together as a family. You know what everyone’s doing. You keep each other accountable. When it comes to a bit bigger than that, you need another layer of administrations.
Things start to get lost. Things start to become a bit impersonal, not so fun to work in. So we keep our hospital small with a capacity [00:49:00] of about two and a half thousand, 3000 deliveries a year. And it’s quite cheap to build. In Australia, you budget building a hospital for at least $1 million per bed.
So when you build a hundred bed hospital, it’s at least a hundred million dollars, at least. And upwards of that so we can build. So a 50 bed hospital we’ve just built in Tanzania. The whole building cost was 1.8 million. Australian. And we are doing all that. So 200 fistula operations a year, outreach work, 15,000 clinic visits a year two and a half thousand, 3000 deliveries a year work.
It just goes on and on. And it’s, and it works. And we get good. You don’t need all the, that’s another thing you learn about healthcare. You can do a lot with a basic healthcare service that’s quite cheap to, to run. And then you have to spend millions to increment your improvements just by a decreasing amount of percentage.
So in Australia, we’re blessed. We’re Wealthy in comparison, we can afford to spend those millions to increase your health outputs by just that fraction of a [00:50:00] percent. But you can do an awful lot. For example, in our hospitals, and it costs 250 Australian dollars, which is around about 180 US dollars.
For a lady to have. All have full clinic visits in the hospital while she’s pregnant, ultrasounds, blood tests delivery in our hospital with a 14% chance of needing a cesarean to have your baby postnatal check. And in two of our hospitals also immunize your child, 250 Australian dollars. You can do a lot with very little.
John Anderson: Andrew, you’ve been very generous with your time. I’ve enjoyed it enormously and I hope lots of people will tune in and enjoy it. In the same way. Thank you.
Andrew Browning: Thank you very much, John.